Even though scientists have been finding new ways to fight cancer, cancer still kills over 9 million people every year worldwide. Genetic mutations are one major cause of cancer that scientists are trying to target therapeutically. Fusion oncogenes are genetic mutations that are especially attractive for cancer therapy because they only occur in cancer cells and not in normal cells, a fact that will cut down on side effects of therapy.
An oncogene is a gene that has the potential to cause cancer. Fusion oncogenes are cancer-causing genes that are made when two separate genes are fused together to make a new gene. Data from The Cancer Genome Atlas has found that fusion oncogenes cause more than 16% of cancers in humans. Finding a way to stop and fix fusion oncogenes could be an important tool to stop these cancers. Scientists think genome editing may be the answer. But how can scientists edit these fusion oncogenes? They use a laboratory technique involving the CRISPR/Cas9 system.
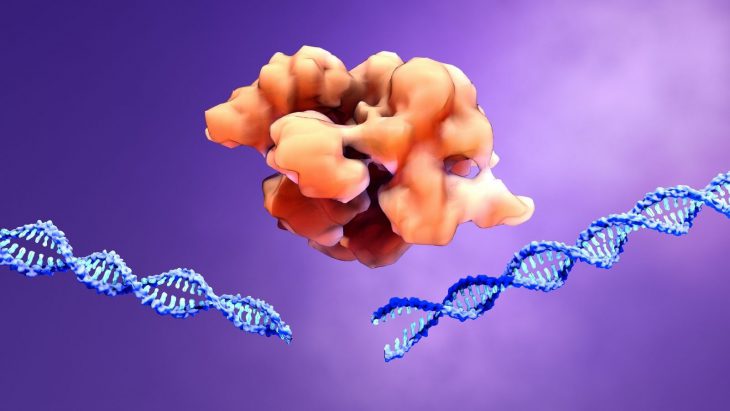
CRISPR/Cas9 is a relatively new technique that can edit DNA in plants and animals. To do this, scientists start with RNA, a molecule that carries the information from DNA to where the cell can read it. The RNA finds the spot in the DNA where the editing should take place and leads the DNA-cutting Cas9 protein there. The Cas9 protein then locks onto the DNA and cuts it, making a break in both DNA strands. New genetic information can be inserted into the broken space. The cell then fixes the break using it’s normal repair mechanisms.
A group of researchers used CRISPR/Cas9 to delete fusion oncogenes in cancer cells without affecting the normal copies of the gene in normal cells. Another study used CRISPR to target fusion oncogenes, but it was considered potentially expensive and inefficient to do clinically because the therapy would have to be personalized to each patient. Because of this, they wanted to do it in a way that isn’t patient-specific.
To target fusion oncogenes, they designed a special kind of RNA to guide the cutting system to areas of the fusion oncogene that didn’t code for anything. These segments are called introns. By snipping the DNA there, they wouldn’t accidentally cut anything important, but would still delete the fusion oncogene.
They first tested this technique outside of a human body, by growing a cell type afflicted with Ewing sarcoma. Ewing sarcoma is a cancer that is caused by fusion oncogenes. Like any gene, fusion oncogenes encode for proteins. The researchers found there was a 4.5-fold decrease in the protein product of the fusion oncogene present in the cells. Even better, the CRISPR/Cas9 system did not interfere with normal non-cancerous cells.
The scientists then looked at how the CRISPR/Cas9 system affected tumor cells’ growth in a Petri dish. They found that there was an increase in tumor cell death when they treated these cells with CRISPR/Cas9. Because this worked for cells on a plate, they wanted to see if this would also work for cells in living organisms.
To do this, the scientists used a procedure called xenograft modeling on laboratory mice. In this procedure, human tumor cells are injected under the skin of mice with compromised immune systems. They let the tumors grow in the mice, and then treated the tumor cells with the special RNA and Cas9. Tumor size was reduced by ~70%. Afterward, they analyzed the now-shrunken tumors and found that none of the remaining tumor cells had any fusion oncogene deletions. This supported the conclusion that all cells whose fusion oncogenes had been deleted had died. The CRISPR/Cas9 was able to control tumor growth in vivo.=
From there, the scientists looked at combining this method with chemotherapy both in cell culture and in mice. The combined effects of doxorubicin (a common chemotherapy drug) and the CRISPR/Cas9 resulted in a larger reduction in tumor size than either doxorubicin treatment or CRISPR/Cas9 treatment alone. Then, they applied this dual treatment method to another cancer that is caused by fusion oncogenes, chronic myeloid leukemia. They found that their new method worked just as well for this cancer, too.
The scientists found a new method that reduces the size of tumors. Even better, it is highly efficient and potentially universal for cancers caused by fusion oncogenes. The CRISPR method was also specific to just cancer cells, leaving healthy cells alone. When healthy cells are spared, it means fewer side effects for patients. Overall, this is a promising method for possible cancer treatment.