Did you know that scientists have actually found cells that can assassinate specific cancerous cells? Scientists have found many ways to treat cancer but have never managed to get rid of it without causing any negative side effects in the patient. The purpose of this study was for scientists to determine if immune cells called Killer T-cells played a significant role in the fight against cancer, and minimize treatment side effects.
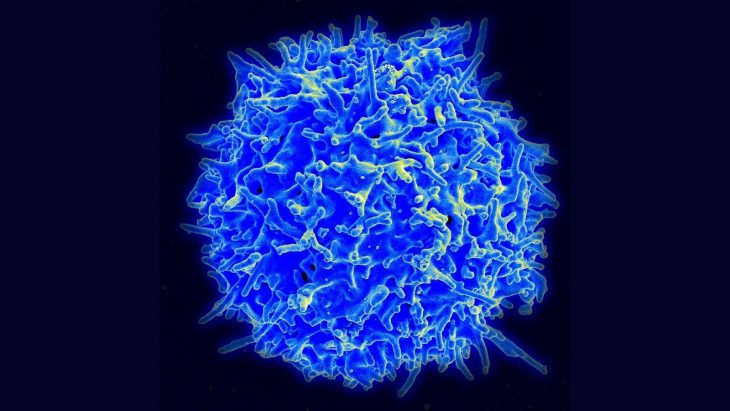
The fight against different cancers is closely tied with the immune system. Killer T-cells are an important part of the immune system because they search for and target pathogens in the body as well as identify tumors. These T-cells can eradicate tumors by causing cell death through different pathways. Cancer cells can also create proteins to block the Killer T-cells from killing them.
Cell death is difficult to induce without negatively affecting healthy cells in the body. That’s what causes the side effects. Chemotherapy kills off cancer cells, but it also kills off healthy cells, causing health issues for patients. Killer T-cells are special because they are already in the body and are an important part of the immune system. The challenge is using them to inhibit tumor growth while still carrying out their other functions, including activating the cells that release antibodies and fight other pathogens and viruses. This research into Killer T-cells is one of the first steps in figuring out how scientists could program cells in the body to target cancer cells and avoid any negative effects to the patient.
Researchers have previously found that nivolumab, a type of immunotherapy, can be used to block these proteins and kill the cancer cells. When the cancer is treated with nivolumab, a process called ferroptosis occurs. Ferroptosis is a type of “programmed cell death,” similar to apoptosis, except during ferroptosis there is a buildup of iron (hence the “ferro-” part of the word) in the cell, and lipids are also broken down.
To determine if ferroptosis could be used in cancer immunotherapy, mice bearing ovarian tumors were treated with a special compound that was expected to cause ferroptosis. After treatment, they measured the iron and lipid levels in the mouse cells. This treatment caused the tumor to shrink. The results also showed increased levels of reactive oxygen species, an immune system function that uses oxygen to kill invaders, in the tumor cell. When these reactive oxygen species increase to a certain level, the cell dies.
The researchers analyzed data from the Cancer Therapeutics Response Portal, comparing different tumor types for what genes they express, called biomarkers, and how sensitive they are to treatment. They discovered 16 biomarkers, which indicate how large the cancer is. All of the biomarkers found were contained in cells that were sensitive to ferroptosis inducers. That means causing ferroptosis would destroy these cancer cell types.
IFNɣ (pronounced “interferon gamma”) is a protein produced by Killer T-cells that is used for cell signaling and can increase reactive oxygen species. When IFNɣ was added along with ferroptosis inducers, cell death was also the result. The researchers also observed increased breakdown of lipids due to oxidation in these cells. This increased oxidation was likely due to the increase in reactive oxygen species.
After carefully analyzing the data, the scientists concluded that the Killer T-cells are strongly associated with lipid peroxidation and also ferroptosis. As the ferroptosis increases in the tumor cells, the immunotherapy becomes more efficient at clearing the tumors. By analyzing which genes were being expressed, the researchers determined that the health of the patients improved with increased IFNɣ protein and killer T cells. They also concluded that killer T cells can successfully inhibit tumor growth. These results contribute to a greater understanding of cancer immunotherapy, reducing side effects for patients.