The world is full of dangerous pathogens, tiny microorganisms that can invade our bodies and cause disease. Our bodies have a natural defense system ready to fight off unwanted invaders: the immune system. The immune system is made up of many different white blood cells that fight off disease. One type of white blood cell, T cells, search out and target invaders by binding to proteins on the surface of infected cells. In recent years, scientists have been trying to use these cells to target tumors in the same way they target pathogens.
Cancer is notorious for being incredibly difficult to treat. Leukemias, cancers that occur within white blood cells, are one of the most persistent and complicated cancers. In recent years, researchers have attempted to use T cells to treat leukemias. They genetically engineered T cells to be used in treatment, naming them as chimeric antigen receptor T cells (CAR T cells). In the past few years, CAR T cell therapy has been incredibly efficient in treating leukemias that arise from B cells, another type of white blood cell.
Despite this success, the use of CAR T cells as a cancer treatment is fraught with difficulty. CAR T cells are produced from a patient’s own cells, which make them time consuming and expensive to make. It can cost up to $475,000 to receive therapy. The side effects of CAR T cell therapy can range between moderate flu like symptoms to organ failure. In some cases, CAR T cell therapy can be life-threatening in patients.
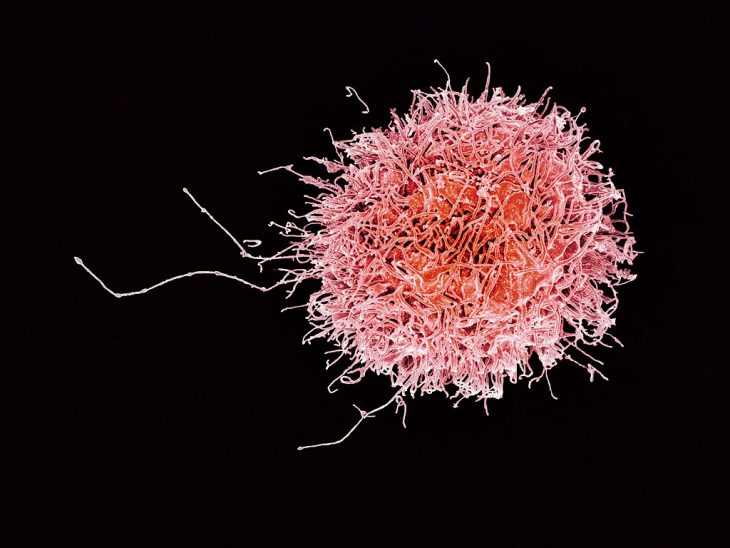
So, what is the solution? CAR T cell therapy can be effective in treating an almost untreatable cancer, but how can researchers make it safer and more efficient? A team of researchers from the University of Texas M.D. Anderson Cancer Center suggested using another form of white blood cell, natural killer cells. Like T cells, natural killer cells search out and kill target cells, although natural killer cells are less specific. Unlike T cells, natural killers don’t have to be produced from the patient and have a better track record in safety as it has fewer negative side effects.
The researchers chose to engineer natural killer cells in the same way as T cells to move past the limitations posed by the use of T cells. They expect that using natural killer cells in place of T cells will reduce the number of toxic effects as well as be easier and cheaper to produce. In this clinical trial, the researchers administered the engineered natural killer cells to patients with leukemia as well as patients with lymphoma, a cancer in the lymphatic system.
Following treatment, 73% of patients saw a decreased tumor size, and eventually 64% of all treated patients had no detectable cancer. Additionally, the response time to the treatment was quick, with patients seeing a decrease in tumor size within the first 30 days.
The researchers also paid close attention to any toxic effects potentially caused by the treatments. Within about a year of treatment, there were no toxic effects observed in patients. The data suggests that natural killer cells are a safe and effective alternative to CAR T cell therapy. Natural killer cell therapy has been found to treat a broader range of cancers and is more cost-effective in comparison to T cell therapy, meaning that it could be more accessible to a greater number of patients. The treatment was also promising in its ability to decrease the size of tumors, potentially introducing an effective treatment for two hard-to-treat cancers, leukemia and lymphoma. Since it is effective and relatively inexpensive, it can become an impactful cancer treatment.